dopamine hydrochloride injection, USP VIAL
Find dopamine hydrochloride injection, USP VIAL medical information:
Find dopamine hydrochloride injection, USP VIAL medical information:
dopamine hydrochloride injection, USP VIAL Quick Finder
17 PATIENT COUNSELING INFORMATION
17 PATIENT COUNSELING INFORMATION
Risk of Tissue Damage
Advise the patient, family, or caregiver to report signs of extravasation urgently [see Warnings and Precautions (5.1)].
Distributed by Hospira, Inc., Lake Forest, IL 60045 USA 
LAB-1154-4.0
Highlights
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use DOPAMINE HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for DOPAMINE HYDROCHLORIDE INJECTION. DOPAMINE HYDROCHLORIDE injection, for intravenous use Initial U.S. Approval: 1974 INDICATIONS AND USAGEDopamine HCl Injection is a catecholamine indicated to improve hemodynamic status in patients in shock. (1) DOSAGE AND ADMINISTRATIONCorrect hypovolemia, acidosis, and hypoxia prior to use. (2.1) Administer in a large vein with an infusion pump preferably in an intensive care setting. (2.1) Recommended starting dosage in adults and pediatric patients is 2 to 5 mcg/kg/minute as a continuous intravenous infusion. Titrate in 5 to 10 mcg/kg/minute increments based on hemodynamic response and tolerability, up to not more than 50 mcg/kg/minute. (2.2) See the Full Prescribing Information for important preparation instructions and drug incompatibilities. (2.1,2.3) DOSAGE FORMS AND STRENGTHSThe following strengths of Dopamine HCL, USP, are supplied in single-dose vials: (3)
CONTRAINDICATIONSDopamine is contraindicated in patients with pheochromocytoma. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe most common adverse reaction is localized vasoconstriction due to extravasation. (6) To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 9/2023 |
Indications and Usage
Dosage and Administration
2 DOSAGE AND ADMINISTRATION
2.1 Preparation and Administration Instructions
Correct Hypovolemia, Acidosis, and Hypoxia
Address hypovolemia, acidosis, and hypoxia before initiating Dopamine HCl Injection. If patient does not respond to therapy, suspect occult hypovolemia. Acidosis may reduce the effectiveness of dopamine [see Warnings and Precautions (5.1)].
Preparation
For the 40‑mg/mL preparation, transfer by aseptic technique the contents containing either 5 mL (200 mg) or 10 mL (400 mg) of Dopamine HCl Injection to either a 250‑mL or a 500‑mL bottle of one of the sterile intravenous solutions listed below:
- •
- 0.9% Sodium Chloride Injection, USP
- •
- 5% Dextrose Injection, USP
- •
- 5% Dextrose and 0.9% Sodium Chloride Injection, USP
- •
- 5% Dextrose and 0.45% Sodium Chloride Injection, USP
- •
- 5% Dextrose and Lactated Ringer’s Injection
- •
- Sodium Lactate Injection, USP 1/6 Molar
- •
- Lactated Ringer’s Injection, USP
The resultant dilutions are summarized in the following chart:
Volume of IV solution | Volume of Dopamine Hydrochloride Injection | |
5 mL | 10 mL | |
250 mL | 800 mcg/mL | 1600 mcg/mL |
500 mL | 400 mcg/mL | 800 mcg/mL |
1000 mL | 200 mcg/mL | 400 mcg/mL |
Dopamine HCl Injection has been found to be stable for 24 hours after dilution in the foregoing intravenous solutions.
Administration
Dopamine HCl Injection is administered (only after dilution) by intravenous infusion.
Administer Dopamine HCl Injection into a large vein [see Warnings and Precautions (5.1)] with the use of an infusion pump preferably in an intensive care setting.
Inspect Dopamine HCl Injection for particulate matter and discoloration prior to administration whenever solution and container permit (the solution is clear, practically colorless). Do not administer if the solution is darker or discolored.
Use higher concentration solutions (e.g., 3200 mcg/mL or 1600 mcg/mL strengths) in patients requiring fluid restriction.
Discontinuation
When discontinuing Dopamine HCl Injection, gradually reduce the infusion rate while expanding blood volume with intravenous fluids [see Warnings and Precautions (5.3)].
2.2 Recommended Dosage
The recommended starting dosage in adults and pediatric patients is 2 to 5 mcg/kg/minute as a continuous intravenous infusion [see Dosage and Administration (2.3)]. Titrate the infusion rate in increments of 5 to 10 mcg/kg/minute based on hemodynamic response and tolerability, but do not exceed 50 mcg/kg/minute.
Infusion rates may be calculated using the following formula:
Infusion Rate (mL/hour) = [Dose (mcg/kg/minute) x Weight (kg) x 60 (minutes/hour)]
Concentration (mcg/mL)
Example calculations for infusion rates are as follows:
Example 1: for a 60 kg person at the recommended initial dose of 2 mcg/kg/minute using a 800 mcg/mL concentration, the infusion rate would be as follows:
Infusion Rate (mL/hour) = [2 (mcg/kg/minute) x 60 (kg) x 60 (minutes/hour)] = 9 (mL/hour)
- 800 (mcg/mL)
Example 2: for a 70 kg person at a dose of 5 mcg/kg/minute using a 1600 mcg/mL concentration, the infusion rate would be as follows:
Infusion Rate (mL/hour) = [5 (mcg/kg/minute) x 70 (kg) x 60 (minutes/hour)] = 13.13 (mL/hour)
- 1600 (mcg/mL)
2.3 Drug Incompatibilities
Dopamine HCl Injection is incompatible with the following products; therefore, avoid simultaneous administration (through the same infusion set):
- •
- Sodium bicarbonate or other alkalinizing substances, because dopamine is inactivated in alkaline solution
- •
- Blood, because of the risk of pseudoagglutination of red cells
- •
- Iron salts
Do not add additional medications in the diluted infusion solution.
Dosage Forms and Strengths
Contraindications
Warnings and Precautions
5 WARNINGS AND PRECAUTIONS
5.1 Tissue Ischemia
Administration of dopamine to patients who are hypotensive from hypovolemia can result in severe peripheral and visceral vasoconstriction, decreased renal perfusion and hypouresis, tissue hypoxia, lactic acidosis, and poor systemic blood flow despite “normal” blood pressure. Address hypovolemia prior to initiating Dopamine HCl Injection [seeDosage and Administration (2.2)].
Gangrene of the extremities has occurred in patients with occlusive vascular disease or who received prolonged or high dose infusions. Monitor for changes to the skin of the extremities in susceptible patients.
Extravasation of Dopamine HCl Injection may cause necrosis and sloughing of surrounding tissue. To reduce the risk of extravasation, infuse into a large vein [see Dosage and Administration (2.1)], check the infusion site frequently for free flow, and monitor for signs of extravasation.
Emergency Treatment of Extravasation
To prevent sloughing and necrosis in areas in which extravasation has occurred, infiltrate the ischemic area as soon as possible, using a syringe with a fine hypodermic needle with:
- •
- 5 to 10 mg of phentolamine mesylate in 10 to 15 mL of 0.9% Sodium Chloride Injection in adults
- •
- 0.1 to 0.2 mg/kg of phentolamine mesylate up to a maximum of 10 mg per dose in pediatric patients.
Sympathetic blockade with phentolamine causes immediate and conspicuous local hyperemic changes if the area is infiltrated within 12 hours.
5.2 Cardiac Arrhythmias
Dopamine may cause arrhythmias. Monitor patients with arrhythmias and treat appropriately.
5.3 Hypotension after Abrupt Discontinuation
Sudden cessation of the infusion may result in marked hypotension. Gradually reduce the infusion rate while expanding blood volume with intravenous fluids.
5.4 Severe Hypersensitivity Reactions due to Sodium Metabisulfite Excipient
Dopamine HCl Injection contains sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
Adverse Reactions
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in the labeling:
- •
- Tissue Ischemia [see Warnings and Precautions (5.1)]
- •
- Cardiac Arrhythmias [see Warnings and Precautions (5.2)]
- •
- Hypotension [see Warnings and Precautions (5.3)]
- •
- Severe Hypersensitivity Reactions [see Warnings and Precautions (5.4)]
The following adverse reactions have been identified during postapproval use of dopamine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac Disorders: anginal pain, palpitation
Gastrointestinal Disorders: nausea, vomiting
Metabolism and Nutrition Disorders: azotemia
Nervous System Disorders: headache, anxiety
Respiratory Disorders: dyspnea
Skin and Subcutaneous Tissue Disorders: piloerection
Vascular Disorders: hypertension
Drug Interactions
7 DRUG INTERACTIONS
- See Table 1 for clinically significant drug interactions with dopamine.
Halogenated Anesthetics | |
Clinical Impact: | Concomitant use may increase cardiac autonomic irritability and can sensitize the myocardium to the action of dopamine which may lead to ventricular arrhythmias and hypertension. |
Intervention: | Monitor cardiac rhythm. |
Examples: | desflurane, enflurane, isoflurane, and sevoflurane. |
MAO Inhibitors | |
Clinical Impact: | Because dopamine is metabolized by monoamine oxidase (MAO), inhibition of this enzyme prolongs and potentiates the effect of dopamine which may result in severe hypertension and cardiac arrhythmia. |
Intervention: | Reduce the recommended starting dosage to no greater than one‑tenth (1/10) of the recommended dose in patients who have been treated with MAO inhibitors within two to three weeks prior to the administration of Dopamine HCl Injection. |
Examples: | isocarboxazid, phenelzine, tranylcypromine, rasagiline, selegiline, linezolid. |
Tricyclic Antidepressants | |
Clinical Impact: | Concomitant use may potentiate the cardiovascular effects of dopamine (e.g., hypertension). |
Intervention: | Monitor blood pressure. |
Examples: | amitriptyline, desipramine, doxepin, imipramine, nortriptyline. |
| |
Clinical Impact: | Concomitant use may result in severe hypertension. |
Intervention: | Monitor blood pressure. |
Examples: | norepinephrine, epinephrine, oxytocin. |
Use in Specific Populations
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no human data with dopamine use in pregnant women. There are risks to the mother and fetus from hypotension associated with shock, which can be fatal if left untreated (see Clinical Considerations). In animal reproduction studies, adverse developmental outcomes were observed with intravenous dopamine HCl administration in pregnant rats during organogenesis at doses, on a mcg/m2 basis, of one‑third the human starting dose of 2 mcg/kg/minute (90 mcg/m2/minute).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies carry some risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2‑4% and 15‑20%, respectively.
Disease-Associated Maternal and/or Embryo/Fetal risk
Hypotension associated with distributive shock, or shock due to reduced cardiac output are medical emergencies in pregnancy which can be fatal if left untreated. Delaying treatment in pregnant women with hypotension associated with distributive shock, or shock due to reduced cardiac output may increase the risk of maternal and fetal morbidity and mortality. Life-sustaining therapy for the pregnant woman should not be withheld due to potential concerns regarding the effects of dopamine on the fetus.
Labor or Delivery
Vasopressor drugs, including dopamine, may cause severe maternal hypertension when used concomitantly with some oxytocic drugs [see Drug Interactions (7)].
Data
Animal Data
Animal reproduction studies in rats and rabbits at dopamine HCl dosages up to 6 mg/kg/day intravenously (on a mcg/m2 basis, one third and two thirds, respectively, the human starting dosage of 2 mcg/kg/minute) during organogenesis produced no detectable teratogenic or embryotoxic effects, although maternal toxicity consisting of mortalities, decreased body weight gain, and pharmacotoxic signs were observed in rats. In a published study, administration of 10 mg/kg/day dopamine HCl (on a mcg/m2 basis, two-thirds the human starting dosage of 2 mcg/kg/minute) to pregnant rats throughout gestation or for 5 days starting on gestation day 10 or 15 resulted in decreased body weight gain, increased mortality, and slight increase in cataract formation among the offspring.
8.2 Lactation
Risk Summary
There are no data regarding the presence of dopamine in human milk, the effects of dopamine on the breastfed infant, or the effects of the drug on milk production.
8.4 Pediatric Use
Dopamine HCl infusions have been used in pediatric patients from birth through adolescence. Most reports in pediatric patients describe dosing that is similar (on a mcg/kg/minute basis) to that used in adults [see Dosage and Administration (2.2)]. Except for vasoconstrictive effects caused by inadvertent infusion of dopamine into the umbilical artery, adverse reactions unique to pediatric patients have not been identified, nor have adverse reactions identified in adults been found to be more common in pediatric patients.
8.5 Geriatric Use
Clinical studies of dopamine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should start at the low end of the dosing range, reflecting the frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
Overdosage
10 OVERDOSAGE
Manifestations of overdosage include excessive blood pressure elevation.
In the case of accidental overdosage, reduce rate of Dopamine HCl Injection administration or temporarily discontinue the dopamine HCl until the overdosage related adverse reactions resolves. Since dopamine’s duration of action is quite short, no additional remedial measures are usually necessary. If these measures fail to resolve the overdosage related adverse reactions, consider using an alpha-adrenergic blocking agent (e.g., phentolamine).
Description
11 DESCRIPTION
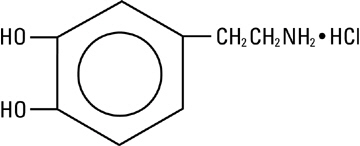
Dopamine, a sympathomimetic amine vasopressor, is the naturally occurring immediate precursor of norepinephrine. Dopamine hydrochloride is a white to off-white crystalline powder, which may have a slight odor of hydrochloric acid. It is freely soluble in water and soluble in alcohol. Dopamine HCl is sensitive to alkalies, iron salts, and oxidizing agents. Chemically it is designated as 4-(2-aminoethyl) pyrocatechol hydrochloride, and its molecular formula is C8H11NO2 • HCl. Dopamine HCl has a molecular weight of 189.64 and it has the following structural formula:
Dopamine (also referred to as 3 hydroxytyramine) is a naturally occurring endogenous catecholamine.
Dopamine hydrochloride injection is a clear, practically colorless, sterile, pyrogen-free, aqueous solution of dopamine HCl for intravenous infusion after dilution. Each milliliter of the 40 mg/mL preparation contains 40 mg of dopamine hydrochloride (equivalent to 32.31 mg of dopamine base). Each milliliter of preparation contains the following: Sodium metabisulfite 9 mg added as an antioxidant; citric acid, anhydrous 10 mg; and sodium citrate, dihydrate 5 mg added as a buffer. May contain additional citric acid and/or sodium citrate for pH adjustment. pH is 3.3 (2.5 to 5.0).
Dopamine must be diluted in an appropriate sterile parenteral solution before intravenous administration [see Dosage and Administration (2.1)].
Clinical Pharmacology
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dopamine is a natural catecholamine formed by the decarboxylation of 3,4 dihydroxyphenylalanine (DOPA). It is a precursor to norepinephrine in noradrenergic nerves and is also a neurotransmitter in certain areas of the central nervous system, especially in the nigrostriatal tract, and in a few peripheral sympathetic nerves.
Dopamine elicits its pharmacological action by activating dopamine D1 and D2 receptors, beta 1 receptors and alpha 1 receptors. The activation of different receptors leading to its effects are dependent on dopamine dose.
12.2 Pharmacodynamics
Dopamine’s onset of action occurs within five minutes of intravenous administration and the duration of action is less than about ten minutes. Dopamine effects are dosage‑dependent.
- •
- At <5 mcg/kg/minute, dopamine HCl activates dopamine D1 and D2 receptors in the renal, mesenteric, and coronary vasculature causing vasodilation.
- •
- At 5 to 10 mcg/kg/minute, dopamine HCl activates beta‑1 receptors enhancing heart rate and contractility.
- •
- At >10 mcg/kg/minute, dopamine HCl activates alpha‑1 receptors causing vasoconstriction and increased blood pressure
12.3 Pharmacokinetics
Distribution
Following intravenous administration, dopamine is widely distributed in the body but does not cross the blood‑brain barrier to a significant extent.
Elimination
The half‑life of dopamine in adults is less than 2 minutes.
Metabolism
About 75% of dopamine is metabolized by monoamine oxidase (MAO) and catechol O‑methyl transferase (COMT) in the liver, kidney, and plasma to the inactive compounds homovanillic acid (HVA) and 3,4‑dihydroxyphenylacetic acid, and about 25% is metabolized to norepinephrine in the adrenergic nerve terminals.
Excretion
About 80% of dopamine is renally excreted as inactive metabolites within 24 hours. Dopamine is stored in vesicles or diffused back into the plasma.
Specific Populations
Pediatric Patients
The reported clearance rate of dopamine in critically ill infants and pediatric patients ranged from 46 to 168 mL/kg/minute, with the higher values seen in the younger patients. The reported apparent volume of distribution in neonates was 0.6 to 4 L/kg, leading to an elimination half life of 5 to 11 minutes.
Nonclinical Toxicology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long term animal studies have not been performed to evaluate the carcinogenic potential of dopamine.
Mutagenesis
Dopamine HCl at doses approaching maximal solubility showed no clear genotoxic potential in the Ames test. Although there was a reproducible dose‑dependent increase in the number of revertant colonies with strains TA100 and TA98, both with and without metabolic activation, the small increase was considered inconclusive evidence of mutagenicity. In the L5178Y TK+/- mouse lymphoma assay, dopamine HCl at the highest concentrations used of 750 mcg/mL without metabolic activation, and 3000 mcg/mL with activation, was toxic and associated with increases in mutant frequencies when compared to untreated and solvent controls; at the lower concentrations no increases over controls were noted.
No clear evidence of clastogenic potential was reported in the in vivo mouse or male rat bone marrow micronucleus test when the animals were treated intravenously with up to 224 mg/kg and 30 mg/kg of dopamine HCl, respectively.
How Supplied/Storage and Handling
16 HOW SUPPLIED/STORAGE AND HANDLING
Dopamine Hydrochloride Injection, USP is a clear, practically colorless solution supplied as follows:
| Unit of Sale | Total Strength/Total Volume (Concentration) |
|---|---|
NDC 0409-5820-01 | 200 mg/5 mL |
NDC 0409-9104-20 | 400 mg/10 mL |
Store at 20°C to 25°C (68°F to 77°F). [See USP Controlled Room Temperature.]
Patient Counseling Information
17 PATIENT COUNSELING INFORMATION
Risk of Tissue Damage
Advise the patient, family, or caregiver to report signs of extravasation urgently [see Warnings and Precautions (5.1)].
Distributed by Hospira, Inc., Lake Forest, IL 60045 USA 
LAB-1154-4.0
Resources
Didn’t find what you were looking for? Contact us.
Chat online with Pfizer Medical Information regarding your inquiry on a Pfizer medicine.
*Contact Medical Information. 9AM-5PM ET Monday to Friday; excluding holidays.
Report Adverse Event
Pfizer Safety
To report an adverse event related to the Pfizer-BioNTech COVID-19 Vaccine, and you are not part of a clinical trial* for this product, click the link below to submit your information:
Pfizer Safety Reporting Site*If you are involved in a clinical trial for this product, adverse events should be reported to your coordinating study site.
If you cannot use the above website, or would like to report an adverse event related to a different Pfizer product, please call Pfizer Safety at (800) 438-1985.
FDA Medwatch
You may also contact the U.S. Food and Drug Administration (FDA) directly to report adverse events or product quality concerns either online at www.fda.gov/medwatch or call (800) 822-7967.